
You Deserve Better: Where to Begin When Considering a Fresh Start for Your Credentialing Process
Presenting a case for better processes requires a sound business case and data. Here's what to measure and how to build your case.
Management thinker Peter Drucker is often quoted as saying that “you can’t manage what you can’t measure.” You’ve probably heard the phrase a thousand times, but have you given any thought to how it applies to those of us responsible for credentialing providers?
Drucker’s message is pretty clear. You can’t know whether or not you are successful unless success is defined and tracked. Without clearly established goals and metrics, you can’t quantify progress or improve your processes to produce the desired outcome. What Drucker seems to really be saying is, “If you can’t measure it, you can’t improve it.”
This, unfortunately is the case today for many professionals responsible for credentialing. Across the industry, many of us are seeking comparative information on credentialing metrics, but because our organizations tend to define things differently and use a variety of methods in collecting data, there are not a lot of metrics available. A lack of industry standards on how credentialing metrics are defined has resulted in a lack of benchmarks for best credentialing practices. This makes it extremely difficult for CVOs and MSOs looking to build cases for improvement. If you can’t show you’re behind the curve, how can you convince management that there’s a need to investment in improvement?
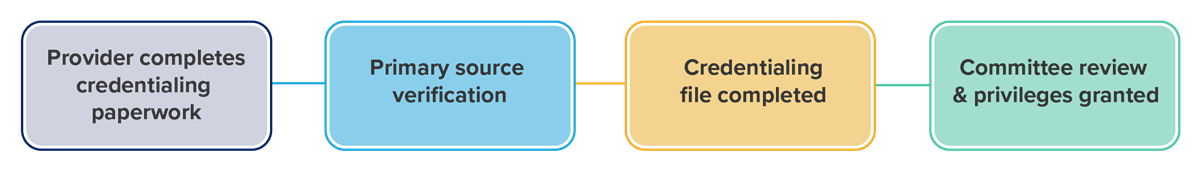
A Typical Credentialing Process:
The industry is making some progress on establishing benchmarks. There are also some methods for measuring your internal processes that can help you pinpoint trouble spots. So, if you’re looking to build a case for freshening up your credentialing, privileging, and enrollment processes, here are five metrics to consider benchmarking this year:
#1 Measure the length of time it takes a provider to submit an application.
Your organization may offer a variety of methods for completing an application such as online, via email or via mail. If so, tracking the time it takes to complete applications via each method can prove the value of one method over another. If you only offer one method for completing an application, it’s still important to track the amount of time it takes for an application to be completed via that method, so that you can learn more about your process. If it takes a provider an excessive amount of time to gather the information requested, you may be requesting too much data or making it too difficult to submit the data. A lot can be learned by simply looking at what’s being requested and how, as well as how the process is actually flowing.
#2 Measure the length of time it takes the credentialing department to begin primary source verification.
The industry has a long way to go before it establishes a standard definition of a completed initial application, but that should not stop your organization from clearly defining when you consider an application complete as this point will serve as a trigger to begin verification. Typically, two elements are required to begin verification: the application must be signed and the critical components of that application must be completed. Additionally, if a provider asks for privileges, they must have signed and submitted their privilege request. The industry is focused on benchmarking the time it takes to perform primary source verification once a completed initial application received, so if you take the same approach, you will be able to benchmark your organization against the industry as soon as this data becomes available.
#3 Measure the number of initial credentialing files returned for additional verification.
Once the initial application is completed, a provider’s file will be gone through with a fine-tooth comb. As education, training, licensure, and employment history are verified, red flags and unanswered questions may surface. When they do – a file will be returned for additional verification. Sometimes files are returned simply because they are incomplete or the applicant failed to follow stated policies and procedures. Regardless of the reason, identifying how many initial files are returned and why can provide important data internally and contribute to establishment of benchmarks on a national level.
#4 Measure the length of time it takes to complete each step of the evaluation and decision-making process all the way through to a board decision.
Once primary source verification is complete an application can be funneled into the evaluation and decision-making process. At this point, your organization should measure the time it takes to complete each incremental step in that process. How long do evaluations take and how quickly are decisions made regarding credentialing and privileging? If you can pinpoint bottlenecks in the overall process, you can prioritize improvements. If this data can be collected and national averages computed, you will also have a starting place for analysis and comparison to other organizations.
#5 Measure the total time it takes from completion of primary source verification to when a provider is able to provide services.
This metric looks at the length of time from the completion of the primary source verification to when a provider can exercise privileges, even if the applicant has only been given temporary privileges. Organizations should capture this data because most want to know who much time they need to budget to complete provider credentialing and enrollment prior to a start date, and whether they should consider allowing certain providers the ability to provide services before the board has made the final decision.
Data Points to Track:
- Date of request of application
- Date application is sent
- Request to return for processing
- Start date of processing
- Review by Dept Chief/Chair/Medical Director
- Committee Dates
- Applicant approval letter/notice
The Value of Metrics
You may be thinking, “My job is hard enough! What good are all these metrics and why do I need them?” Well, without them, your job will only get tougher. A lack of metrics means:
- You can’t show you need additional staffing.
- You can’t show you need additional tools, such as software to do your job effectively.
- You can’t articulate the relationship between credentialing and revenue cycle management.
- You can’t show your impact on reducing cash at risk.
- You can’t show the impact of having to rush providers through credentialing and getting late notice on starting providers.
With clearly established goals and metrics, you’ll be able to benchmark performance, identify and quantify progress improvements and begin producing desired outcomes. Keep these words in mind: “When you measure it, you can improve it!”
Need help?
If you need help building a case for freshening up your credentialing, privileging, and enrollment processes and telling your story, reach out to VerityStream. Our team is in a unique position to offer advice as 2,500 hospitals and 1,300 outpatient facilities currently rely on our credentialing, privileging, enrollment, and evaluation solutions. We’d love to help you too!
