
For the past six years, VerityStream has been conducting an annual survey on provider enrollment. Our goal is to uncover the top provider enrollment trends so that organizations like yours can better evaluate and manage their processes. This year, we surveyed over 500 Provider Enrollment professionals, the majority of whom were part of a physician or medical practice who are standalone, a corporate location of a health system (including health system-based CBOs), and hospitals that are part of a health system.
Responses revealed that the No Surprises Act is having a big impact on workloads and processes. In this post, we’ll dive into the requirements of the No Surprises Act and how they are impacting credentialing experts.
What is the No Surprises Act?
The No Surprises Act protects people covered under group and individual health plans from receiving surprise medical bills when they receive most emergency services, non-emergency services from out-of-network providers at in-network facilities, and services from out-of-network air ambulance service providers.
Impact of the No Surprises Act
Congress passed the No Surprises Act as part of the Consolidated Appropriations Act to eliminate surprise medical bills. The act contains requirements related to price transparency and provider directories that impact health plans. There are four new compliance tasks associated with the No Surprises Act that are impacting credentialing and enrollment professionals. These include the need to:
- Provide an accurate public-facing provider directory database
- Verify the provider directory database at least once every 90 days
- Update the provider directory within two business days of a provider's change in information
- Respond to inquiries regarding a provider's or facility's network status within one business day, in or out of network
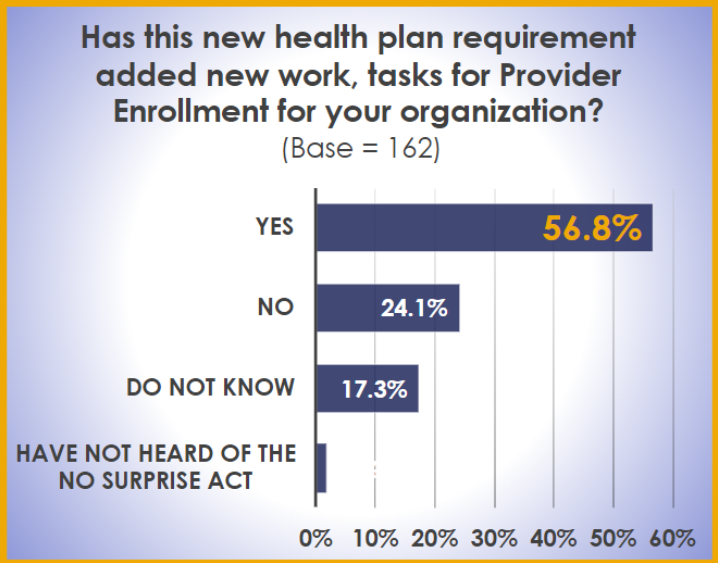
It’s a large undertaking, so we sought to understand how the new requirements are impacting credentialing and enrollment professionals. It comes as no surprise that over half the respondents shared that these four new compliance tasks are adding new work to their day-to-day.
Those who were impacted by The Surprises Act were also asked to estimate how much time is being spent on the newly required tasks.
- 39.1% spend between 3-5 hours per week
- 31.5% spend between 0-2 hours per week
- 16.3% spend more than 8 hours per week
- 13% spend between 6-8 hours per week
Interestingly enough, while enrollment organizations have seen an increase in the hours attributed to The No Surprises Act, 74.7% indicated that they have not added any new Full Time Employees (FTEs) to their organization, making it more important than ever to have automation in place to complete the work. Credentialing professionals will continue to work through a new system with many unanswered questions for the foreseeable future, as we are still waiting for The Centers for Medicare & Medicaid Services (CMS) to provide their rules and regulations.
In Summary
In summary, the demands of the No Surprises Act are challenging credentialing and enrollment professionals to do more with their existing resources. Directory accuracy has always been an important aspect of information to the public, but ensuring accuracy is now more critical than ever before. And without additional resources, our experts will need to lean heavily into developing the most efficient process as possible to complete the work.
This year’s annual survey uncovered many additional findings on pending claims, integrating with external services such as CAQH or PECOS and meaning provider data. Get the full scoop by downloading the report, or watch the webinar uncovering the results. We hope you find this information as valuable as we did, and if you have any questions, we’re only a phone call away.
